Medication errors can occur at any time during therapy. The most common medication error is a timing error, which means the time interval between dosage forms is not followed properly. The second most common error is an omission error, which means the patient doesn’t receive the scheduled dose of medication. Other errors include prescribing errors, wrong dose errors, wrong preparation errors, wrong administration errors, deteriorated drug errors, monitoring errors, compliance errors, duplication errors, and unauthorized drug errors.
Medication errors are categorized by the NCC MERP index according to their severity
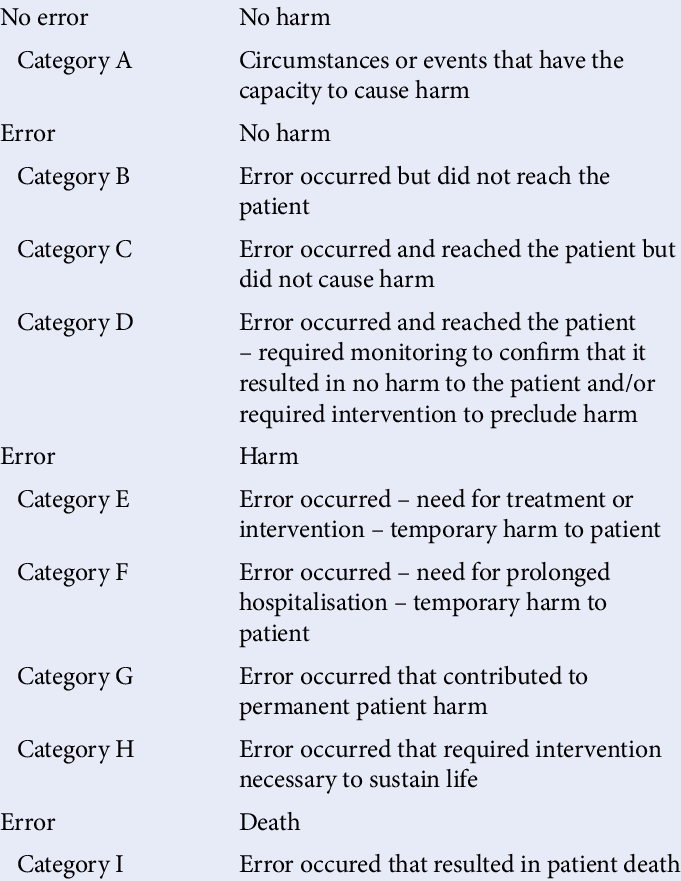
The consequences of medication errors range from no harm to death. Medication errors can significantly affect patient safety.
Adverse drug reactions can result from the use of the wrong medications or incorrect dosages, leading to minor to severe side effects. Delayed or ineffective treatment due to patients not taking their medicine properly can result in the worsening of the patient’s condition and lead to complications.
Medication non-adherence may occur when patients are confused about their medications or fear experiencing adverse effects, leading to improper medication intake.
Medication errors can increase healthcare costs by necessitating additional medical interventions, hospital readmissions, or longer hospital stays, resulting in increased costs for both patients and the healthcare system.
Patient safety can be improved by preventing medication errors through strategies such as medication reconciliation, staff training, standardizing processes, and patient education.


